The air in the hospital corridor was thick with the scent of antiseptic, but the real danger was invisible. A young woman, barely thirty, lay in isolation, her body ravaged by an infection that laughed in the face of modern medicine. The bacteria invading her bloodstream carried a genetic mutation that rendered every antibiotic in the hospital's arsenal useless. This wasn't some dystopian fiction—it was happening in a major urban medical center last Tuesday. Her story is becoming frighteningly common as we enter what some epidemiologists call "the post-antibiotic era."
Our miracle drugs are failing. The antibiotics that once saved millions now meet resistance at nearly every turn. The World Health Organization warns that routine surgeries could become deadly within our lifetime if current trends continue. What went wrong? The answer lies in our reckless overuse of these precious medications—in hospitals, farms, and households across the globe.
Walk into any clinic with a sore throat, and you'll likely leave with an antibiotic prescription—despite viruses causing most upper respiratory infections. Farmers feed antibiotics to healthy livestock to promote growth. Pharmaceutical companies marketed these drugs aggressively, creating generations who believe antibiotics cure everything. Meanwhile, bacteria evolved. They always do. With each unnecessary dose, we've trained our microscopic enemies to survive.
The numbers tell a horrifying story. Antimicrobial resistance claims at least 1.27 million lives annually according to recent Lancet data—more than HIV or malaria. By 2050, that figure could reach 10 million. Common infections like pneumonia, tuberculosis, and foodborne illnesses are becoming untreatable in certain regions. Gonorrhea—once easily cured—now has strains resistant to all known antibiotics. Even last-resort drugs like colistin, previously considered too toxic for human use, are encountering resistance.
Modern medicine stands on the brink of collapse. Without effective antibiotics, chemotherapy becomes impossibly dangerous, organ transplants untenable, and C-sections potentially lethal. The very infrastructure of healthcare depends on our ability to control infections. Yet few politicians prioritize this slow-moving crisis, and pharmaceutical companies abandoned antibiotic development decades ago—the drugs weren't profitable enough.
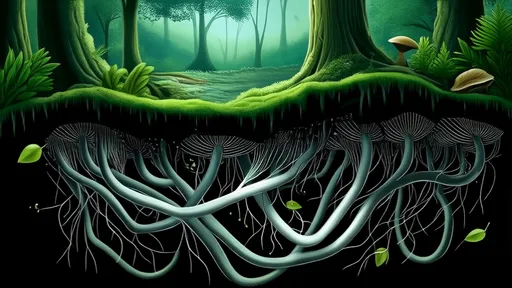
There's grim irony in our predicament. Alexander Fleming, who discovered penicillin, warned about resistance in his 1945 Nobel lecture. We didn't listen. Now, superbugs bred in hospital pipes, factory farms, and overmedicated patients circle like sharks. Some already inhabit healthy people's guts silently, waiting for weakened immune systems to attack.
Hope isn't lost—but time is running short. Researchers explore phage therapy, CRISPR-based solutions, and novel compounds from unlikely sources like soil microbes and frog skin. Hospitals implement stewardship programs to curb unnecessary prescriptions. The European Union banned antibiotic growth promoters in livestock. Public awareness grows, albeit slowly.
Your actions matter. Never demand antibiotics for viral illnesses. Complete every prescribed course. Avoid antibacterial soaps. Choose antibiotic-free meat. These small acts collectively slow resistance. The alternative is unthinkable—a world where a scraped knee could kill, and medicine's greatest achievement becomes obsolete.
That young woman in isolation? She survived—barely. Doctors resurrected an abandoned 1940s drug with terrible side effects as a last resort. Her case represents both our failure and our fragile hope. The superbugs are coming. Whether they overrun us depends on what we do today.
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025