For years, scientists have been puzzled by the mysterious behavior of cancer cells, particularly their tendency to spread more aggressively at night. Recent research has uncovered startling evidence that suggests metastatic activity—the process by which cancer spreads to distant organs—peaks during nighttime hours. This discovery challenges long-held assumptions about the constant, unrelenting nature of cancer progression and opens new avenues for timed therapies.
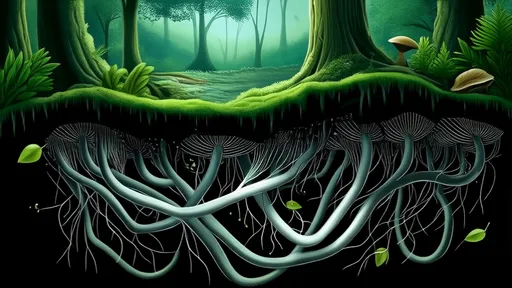
The human body operates on a circadian rhythm, an internal clock that regulates everything from sleep cycles to hormone production. Emerging studies indicate that cancer cells may hijack these biological rhythms to facilitate their spread. While healthy cells follow predictable patterns of activity and rest, malignant cells appear to exploit the body's nocturnal state, using cover of darkness to break away from primary tumors and invade other tissues.
Blood flow dynamics may play a crucial role in this nightly migration. Research shows that circulating tumor cells (CTCs)—the rogue cells that travel through the bloodstream to establish new tumors—are significantly more abundant during sleep. The body's resting state creates ideal conditions for these cells to detach and circulate, as blood vessels become more permeable and certain hormones that promote cell mobility reach their peak levels.
Another factor involves the immune system's circadian fluctuations. Our natural defense mechanisms follow daily cycles, with certain immune cells being less active at night. This temporary lull in immune surveillance might provide cancer cells with a window of opportunity to evade detection as they travel through the bloodstream or lymphatic system. The cover of biological darkness essentially gives metastatic cells a head start before the immune system's daytime reinforcements arrive.
The hormonal environment after dark further facilitates cancer's spread. Melatonin, often called the sleep hormone, shows complex interactions with cancer cells. While it demonstrates some anti-cancer properties, its presence during nighttime may inadvertently create conditions favorable for metastasis through indirect mechanisms. Simultaneously, stress hormones like cortisol that typically decrease at night might normally suppress cancer spread during daylight hours.
Cancer cells themselves exhibit time-dependent gene expression. The same genes that control a cell's internal clock also regulate genes involved in invasion and metastasis. At night, these genes shift their activity patterns, essentially putting cancer cells into "travel mode." This includes increased production of enzymes that help break through tissue barriers and enhanced ability to survive in the bloodstream—both critical steps in the metastatic cascade.
This nocturnal pattern of metastasis has profound implications for cancer treatment. Current therapies are typically administered without regard to the time of day, potentially missing optimal windows for intervention. Chronotherapy—the practice of timing treatments to align with biological rhythms—could dramatically improve outcomes. Some studies already show that administering certain chemotherapy drugs at specific times can reduce side effects while increasing effectiveness against cancer cells.
The discovery of cancer's nightly activities also suggests new diagnostic possibilities. Blood tests for circulating tumor cells might be more effective if performed during nighttime hours when these cells are most active. Similarly, monitoring patients for metastatic risk could involve assessing nighttime biological markers rather than relying solely on daytime measurements.
While these findings represent a significant breakthrough, many questions remain unanswered. Researchers are still working to understand why different cancers might follow varied temporal patterns and how factors like sleep disruption or night-shift work affect metastatic risk. The complex interplay between the body's master clock in the brain and peripheral clocks in individual organs adds another layer of complexity to this emerging field of chrono-oncology.
This new understanding fundamentally changes how we view cancer progression. Rather than imagining tumor cells as constantly active threats, we must now consider them as sophisticated adversaries that carefully time their attacks. As research continues, the medical community may need to rethink everything from hospital routines to treatment schedules, potentially ushering in a new era of cancer care synchronized with the body's natural rhythms.
The implications extend beyond treatment timing to basic cancer biology. If metastasis proves to be dominantly a nocturnal process, it could explain why some screening methods have limitations and why certain treatments fail to prevent spread. This paradigm shift might eventually lead to entirely new classes of drugs designed specifically to disrupt cancer's nightly activities, potentially saving countless lives by preventing metastasis before it begins.
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025