The human body often sends subtle distress signals before catastrophic health events occur. When it comes to sudden cardiac death—the medical community's most terrifying specter—these warning signs frequently manifest in the preceding 24 hours, yet most victims dismiss them as minor discomforts. Understanding these physiological cries for help could mean the difference between life and death.
A crushing fatigue unlike ordinary tiredness often appears as the first harbinger. This isn't the pleasant exhaustion after a good workout or the sleepy haze of a late night. Victims describe it as a leaden weakness permeating their bones, making simple tasks like climbing stairs feel like marathon efforts. The fatigue carries a peculiar quality—it feels wrong in ways the sufferer can't articulate, as if their very cells are screaming under some invisible burden.
Many who narrowly escaped sudden death report experiencing unexplained sweating episodes during their final healthy day. The sweat often has a cold, clammy texture dissimilar to normal perspiration from heat or exertion. It breaks out suddenly, drenching shirts and sheets without apparent cause. This "death sweat" leaves victims confused, sometimes changing clothes multiple times while never connecting the symptom to their impending cardiac crisis.
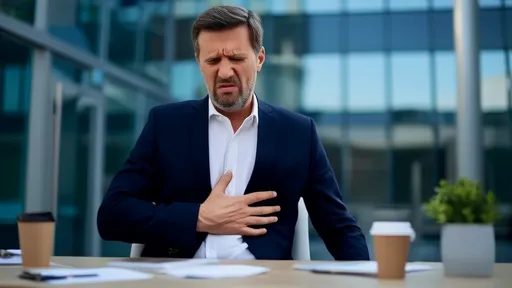
The chest discomfort preceding sudden cardiac death rarely presents as dramatic Hollywood-style heart attacks. More commonly, people describe a peculiar pressure—not quite pain—like an invisible hand squeezing their sternum intermittently. Some perceive it as indigestion that antacids won't relieve, others as a strange fullness when they haven't eaten. This sensation tends to wax and wane, lulling victims into false security until the final, fatal arrhythmia strikes.
Subtle neurological changes frequently occur as the heart's declining function starves the brain of oxygen. Many survivors recall a peculiar mental fog—forgetting simple words, struggling with basic math, or experiencing brief episodes of disorientation in familiar surroundings. These cognitive glitches are often mistaken for stress or fatigue, but they represent the brain operating on dwindling oxygen reserves as the heart loses its rhythm.
Nearly 60% of sudden cardiac death victims experience unusual breathing patterns in their last day. Some report feeling winded after minimal activity, others describe episodes of inexplicable air hunger—the unsettling sensation of not getting enough oxygen despite normal breathing. A smaller subset experiences brief periods of rapid, shallow panting unrelated to exertion or anxiety. These respiratory warnings reflect the heart's diminishing capacity to oxygenate blood.
The gastrointestinal system often sounds alarms through mysterious nausea without vomiting. This isn't food poisoning or stomach flu nausea, but rather a persistent, low-grade queasiness that comes in waves. Many victims report losing their appetite completely, with favorite foods suddenly seeming repulsive. Autopsies frequently reveal this coincides with the beginning of myocardial cell death—the heart muscle literally digesting itself from oxygen deprivation.
Perhaps most chilling are the accounts of impending doom described by survivors. This isn't metaphorical anxiety but a visceral, bone-deep certainty that something catastrophic approaches. Neurologists speculate this arises from the limbic system detecting fatal irregularities in vital signs. Victims suddenly make unexpected phone calls to loved ones, give away possessions, or utter strange farewells—their subconscious recognizing what their conscious mind denies.
Sleep disturbances the night before prove particularly ominous. Many victims experience unexplained nighttime awakenings with a racing heart, others report terrifying dreams of suffocation or being crushed. Cardiologists note these often coincide with dangerous arrhythmias that spontaneously correct—temporary malfunctions that foreshadow the final, fatal episode. The body's circadian rhythms somehow sense the coming storm.
What makes these signals so deadly is their deceptive subtlety. Unlike dramatic heart attacks with collapsing victims clutching their chests, pre-sudden death symptoms often mimic mundane ailments. The pressure gets dismissed as heartburn, the fatigue as overwork, the nausea as a stomach bug. Even medical professionals occasionally miss the patterns unless specifically trained to connect these dots. Yet in retrospect, the body's warnings seem glaringly obvious.
Modern cardiology emphasizes that clusters of these symptoms hold more predictive power than single complaints. A middle-aged man with unexplained sweating plus chest pressure plus sudden fatigue has perhaps minutes to seek help. Yet cultural narratives about toughness, busy schedules that ignore self-care, and healthcare systems that reward downplaying symptoms all conspire to make people ignore these warnings until it's too late.
The cruelest aspect may be timing. These signals typically appear just hours before death—too late for preventative measures but early enough that emergency intervention could save lives if recognized. This narrow window turns ordinary people into unwitting time bombs, carrying fatal flaws they don't comprehend until the final moment. Yet awareness of these signals, disseminated broadly, could rewrite thousands of fatal endings annually.
Survivors often describe their experience as the body whispering before it screams. The tragedy is how few understand the language of those whispers until death teaches its harsh vocabulary. In an era of medical miracles, perhaps our greatest lifesaving tool isn't some advanced technology, but simply learning to heed our flesh's quiet warnings before they become final words.
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025
By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025

By /Jun 7, 2025